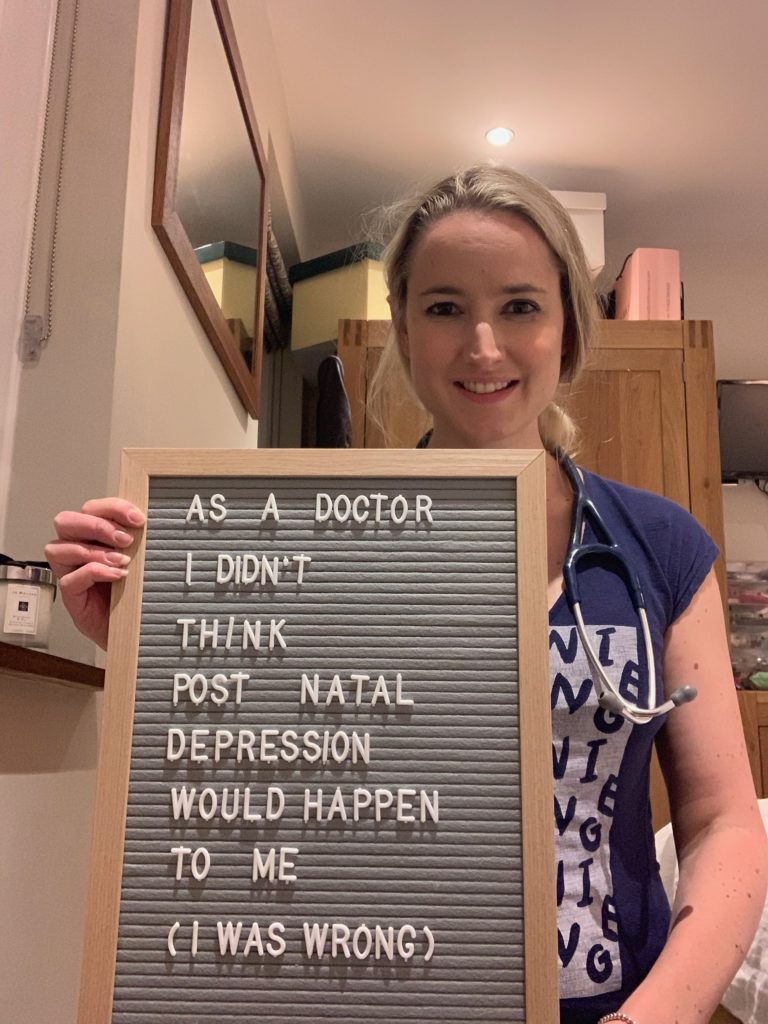
When I started this blog, my goal was to give a totally honest account of motherhood. Whereas my style is generally to try and be truthful whilst also aiming to see the funny side of most things, I have come to realise that being honest also means writing about the not-so-funny things that can happen on one’s motherhood journey.
From just reading the title of this post, you will know that it is about post natal depression (PND). This is obviously not a topic that can really be joked about, and neither should it be. I wasn’t intending to write about my experiences with PND because I thought the subject matter would look a bit out of place on my usually funny blog and also because I didn’t really feel as though I wanted to share my ordeal with the whole world. However, since starting the Instagram account that goes with this blog (check this out by clicking here), I have engaged with a lot of fellow mothers and have read and commented on other people’s accounts of PND. As a result, many people have mentioned that they would be interested to read my story.
As I said in this title, I never thought post natal depression would affect me. I don’t know why exactly I thought this- after all, it is common amongst post partum women (more than 1 in 10 will experience it within a year of giving birth(1)), especially those who have a family history of the condition. My maternal grandmother suffered from particularly bad post-natal depression after all three of her children were born. Given this, I’m not sure exactly why I was so complacent. I suppose I thought that because I am a doctor, there was no way I wouldn’t spot the signs and symptoms early. I also consider myself to be a positive person most of the time, and so I had no reason to think I would be affected by any form of depression during what was supposed to be a very happy time in my life.
Following the birth of my first son Henry in September 2017, I had felt fine. I was lucky to have several friends who all had babies of a similar age and so I got out and about regularly with friends I had known for years and that I could easily spend time with and relate to. I loved motherhood so much and wanted another child as soon as possible. We were very fortunate that we conceived our second child relatively quickly, and we soon discovered that we were expecting again for November 2018. This meant that the children were only going to be 13.5 months apart in age. Everything seemed to be going well. However, between discovering I was pregnant for the second time and having Edward, my second child, quite a lot happened.
I returned to work full time (as an anaesthetic registrar on the NHS in England) in June 2018. Unfortunately in between me finishing work last time to have Henry and returning afterwards quite a few of my colleagues had fallen ill- about 3-4 had been diagnosed with life-changing illnesses. Many of them were only a little bit older than I was (mostly early to mid thirties) and the others were certainly not old by any stretch of the imagination. This had understandably caused quite a bit of shock and anxiety amongst all of us at work. As doctors you often have this weird sense of invincibility- you see sick people all the time but you always assume that it will never happen to you. When it happens to you or someone you know, it is always a real shock. Secondly, I was back to working a full-time NHS rota (this is a lot of hours and includes night shifts and weekend shifts) with a 10 month old child who still wasn’t sleeping through the night. The lack of sleep on top of the long hours and an advancing pregnancy was not especially easy to handle. By the September I was off work with a flu-like illness that didn’t improve with bed rest. Unfortunately the following week I was admitted to hospital with sepsis secondary to pneumonia. Luckily I recovered after treatment with intravenous antibiotics and intravenous fluids. I was advised not to return to work before I started my second maternity leave after I was discharged from hospital, but I did (doctors tend to be stupid like that, but I guess I didn’t want anyone to think I was slacking just because I was pregnant). Henry had started nursery in the September and as anyone with a kid in nursery knows, nurseries are a breeding ground for disease. As a result, Henry had been unwell a few times and so this hadn’t helped his sleeping at all. When I finally finished work for maternity leave, it’s safe to say that I was exhausted.
I’ve already told you about Edward’s birth (you can read about it here if you haven’t already). He arrived on Saturday November 17th 2018 at 20.25. In the month-or-so following his birth, everything seemed fine. I was extremely lucky that Henry was at nursery in the day and so I had plenty of time to bond with Edward. Henry also started sleeping a lot better after Edward was born (I don’t know if this was just a coincidence). Edward was a very easy baby as well- he was a good weight at birth and fed very well. I didn’t even hate breastfeeding him (I hated it with Henry). All in all, it seemed as though everything was going swimmingly.
I think it was around mid-December when things started going wrong in my mind. I wouldn’t say I felt depressed exactly to begin with; rather, I felt increasingly anxious. I was scared that something was going to happen to me and that I would leave my two young children behind without a mother. I thought this was all just hormonal and as a result of the worry caused by several of my colleagues having become unwell, and that eventually it would disappear on its own. After all, I had heard that some degree of anxiety following birth was common and not necessarily cause for concern. However, things gradually started escalating. I soon became convinced that something was wrong with me. For some reason, I became fixated on the belief that I had somehow contracted a blood borne virus, such as HIV. Because I come into frequent contact with blood as part of my job, I convinced myself that I must have been stuck with an infected needle without realising it, or that I must have been splashed with infected blood at one time or another. After all, I was frequently involved in managing major traumas and so there was always blood flying around the place. Before long, I was spending almost all of my free time looking up risk factors for blood borne viruses and convincing myself I had one. Gradually, I started to become more and more disinterested in socialising and pursuing other hobbies, which is not like me at all. It wasn’t long before I was mostly staying in the house worrying all day. I started experiencing physical symptoms of anxiety such as my heart racing at rest. It became all consuming. I had also started drinking heavily in the evenings (which is also not like me. Yes I enjoy a good time and this sometimes involves too much alcohol, but generally speaking, I rarely drink during the week or at home). I don’t think that this was because I had an addiction to alcohol, but rather because I felt like it would help me to relax. Of course alcohol does not help with anxiety at all; rather, it worsens it in the long-term. So this was probably adding to my problems.
My husband started to notice that things weren’t right over the Christmas period and started to suggest that I should see a doctor. When the health visitor came to do a routine follow-up she agreed with him. After I saw a close friend at a Christmas party and thought I had been acting normally, she sent me a text message asking me if I was ok because “you didn’t seem yourself.” It seemed to have become apparent to quite a few people who knew me well that something was amiss. At this point, I hadn’t accepted or acknowledged that anything was wrong and so I didn’t visit the doctor. Over the Christmas period, one colleague passed away. By January, things started to escalate rapidly. I slowly became completely consumed with the idea that I was sick. My husband essentially forced me to see a doctor when, one morning, I told him he couldn’t touch me because my blood was poisoned and he would get ill if he did. We tested my blood with a home HIV test and it was negative. Yet still I was convinced that the test was wrong and I was infected. He called the doctors’ surgery and told them what was going on. They wanted to see me straight away.
I was completely honest with what had been going on when I saw the doctor. I told them about the delusional beliefs I had, about the drinking, and the loss of interest in daily activities. They screened me for suicidal ideation (which luckily I did not have. Throughout the whole process I was highly anxious and delusional about being sick but I am glad to say that I never felt suicidal). I was started on some anti-depressants and told to return shortly afterwards for a follow-up appointment.
By this point, I had definitely accepted that I was mentally ill and I had insight into the fact that what I was experiencing was not normal. Luckily for me, the antidepressants worked and soon I was able to accept the fact that the ideas I had been having were completely delusional. The anxiety etc hadn’t completely gone, but things did improve rapidly. I also made a conscious effort to stop drinking as much (this wasn’t easy, but I realised things had to change quickly here and being on the antidepressants helped with the anxiety that I had been using alcohol to try and counteract). Unfortunately, with all this going on I stopped breastfeeding, which I didn’t really want to do so early but I had to focus on getting better and doing what was right for me and the family at the time. By the time I went back for the follow-up, I was able to confirm that all of the things I had been saying about being sick were completely not true. The doctor told me that I should be on the anti-depressants for at least 6 months. They advised that I organise some counselling (but I am highly ashamed to say that I never did this, although in hindsight I feel like I definitely should have).
I am very lucky that I managed to get off the antidepressants after 6 months, although it can take a lot longer for people to wean down medication. As a doctor, I never thought that things would get so out of control for me. I always thought I would recognise and acknowledge the symptoms of PND and get help early if I experienced them. However, when you are the one with irrational thoughts and beliefs that isn’t always easy to do. Despite not having any issues after my first baby, I had significant ones after my second. Every pregnancy and post partum period can be different. I wish I had listened to those closest to me at the time when they first raised concerns. I now know that PND can manifest in different ways. For instance, mine began as a more anxiety/OCD type thing, but as it escalated, I did become depressed in addition. Luckily, nothing too terrible resulted from my ordeal, and I realise that my case is by no means the worst, but PND can be very serious and in the worst case scenario can even cost lives (that of the mother and/or the baby). If you or a loved one is concerned about PND, please speak to your doctor or health visitor as soon as possible.
It took quite a lot for me to put all of this in writing, but I really hope it may help someone somewhere to recognise the signs and symptoms of PND and to help someone who may be suffering from it. I have tried to be honest with my friends about my experiences with the view that if I can talk about it then hopefully none of them will bottle anything like this up. At the end of the day, PND is a common illness and it is nothing to be ashamed of. It can happen to all of us, even doctors.
Facts About PND (1)
PND is a form of depression that can affect women or even their partners within the year following the birth of a child. Although it is quite common to experience “baby blues” in the first 2 weeks after giving birth, any symptoms suggestive of depression or anxiety that persist beyond this time or begin later may be PND. PND may start at any point during the first year after childbirth. PND can be insidious in onset and so many people may not realise that they or a loved one may be suffering from it. Below are some signs (as per the NHS UK website) suggestive of PND:
“A persistent feeling of sadness and low mood”
Lack of enjoyment and loss of interest in activities
Lack of energy/feeling tired all the time
Difficulty sleeping at night
Feeling tired or wanting to sleep during the day
Problems bonding with your baby
Withdrawing from contact with others e.g. friends
Impaired concentration
Difficulty with making decisions
Frightening/irrational thoughts- e.g. thoughts about hurting yourself or your baby
If you notice any of these signs in yourself or a loved one, then please contact your GP or health visitor without delay. There are a variety of treatment options for PND available, including counselling, cognitive behavioural therapy and pharmacological treatments such as antidepressants. Please do not suffer in silence.
References Used in this Blog Post
- Post Natal Depression available at https://www.nhs.uk/conditions/post-natal-depression/ accessed 18th September 2019
What an amazing post, I’m sure reading it will help many people. So glad to hear you are feeling better now x